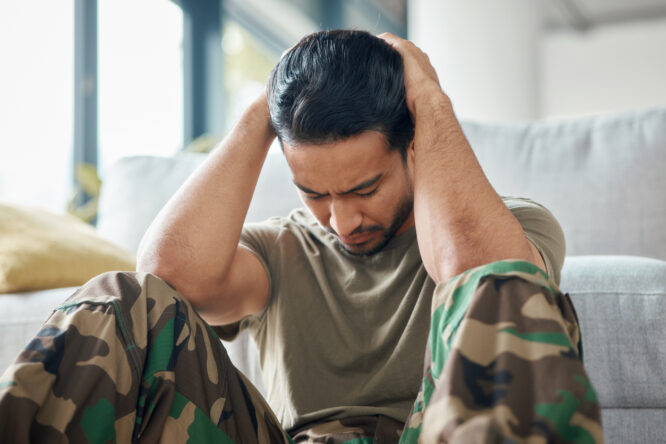
When veterans return home, people often focus on the things they can see.

It’s all about the uniform, the medals, the physical injuries if there are any. Of course, many of the deepest wounds aren’t seen at all. Emotional scars, mental health struggles, and the loss of a clear purpose after service can all weigh heavily, often in silence. While there’s growing awareness of these challenges, veterans still face misunderstanding, isolation, and a system that doesn’t always meet their needs. Here are some of the realities veterans often carry with them, and what can actually help.
1. They carry a deep sense of responsibility that never fully shuts off.

Many veterans spent years in environments where the stakes were high and mistakes could cost lives. That level of pressure doesn’t just disappear when they come home. It often shows up as hypervigilance or feeling like they can never fully relax. What they need isn’t to be told to “just let it go.” They need understanding that their alertness comes from survival, not stubbornness. Support that helps them gradually feel safe again can make a real difference.
2. They often struggle with survivor’s guilt, even when no one talks about it.

Survivor’s guilt isn’t always obvious. It can look like withdrawal, self-doubt, or a reluctance to enjoy life. Veterans may question why they made it home when other people didn’t, and that quiet guilt can linger for years. They don’t need pity. They need space to express these feelings without judgement. Sometimes, just being allowed to say, “I feel this, and I don’t know what to do with it,” can be healing in itself.
3. The transition to civilian life can feel like losing part of their identity.

Military service is more than a job—it’s a lifestyle, a structure, and often a sense of belonging. Coming home can feel like being dropped into a world that no longer makes sense or doesn’t fit. Servicemen and women need more than just job training or resume help. They need community, purpose, and people who see them as whole humans, not just a former rank or title.
4. PTSD can show up in subtle ways.

Not every veteran with PTSD has dramatic flashbacks. It can appear as irritability, avoidance, anxiety, or emotional numbness. Because these signs can be misunderstood, they’re often written off as personality issues rather than symptoms. Understanding the many faces of PTSD is key to offering support that actually helps. They need people who don’t flinch, panic, or judge when trauma shows up in unexpected ways.
5. They may downplay their needs because they don’t want to be a burden.

Military culture often values strength, endurance, and putting other people first. That mindset doesn’t disappear after discharge. Many veterans are hesitant to ask for help because they don’t want to be seen as weak or needy. Sometimes, what they really need is someone to notice they’re struggling, and gently offer support without waiting for them to ask. They need to know they’re allowed to be cared for, too.
6. They can feel isolated, even when surrounded by people.

Unless you’ve served, it’s hard to fully understand what veterans have lived through. This can create an invisible wall between them and the civilian world, making it hard to feel truly seen or understood. They need spaces where they can be real without having to explain or defend their experiences. Peer support, veteran groups, and trauma-informed care can be powerful sources of connection.
7. Flashbacks and triggers can hit when they least expect it.

A sound, a smell, or even a moment of silence can bring memories flooding back. Triggers are unpredictable, and they can leave veterans feeling ungrounded, embarrassed, or even ashamed. They don’t need anyone to fix it. They just need those around them to respond with calm, compassion, and no judgement. Knowing someone won’t overreact helps create a sense of safety they can lean on.
8. Nightmares and disrupted sleep are incredibly common.

Many veterans struggle with sleep—not just falling asleep, but staying asleep without waking in a panic. Nightmares can replay old events or leave them waking up tense and exhausted, night after night. They need more than just advice to “get better rest.” They need trauma-informed treatment options, understanding from loved ones, and patience with their sleep struggles, not pressure to push through.
9. Substance use can be a way to numb what they can’t put into words.

Alcohol or drug use doesn’t always come from recklessness. Often, it’s a coping mechanism for things they don’t feel safe talking about or haven’t been given the tools to manage in healthier ways. Instead of judgement, they need access to compassionate support that addresses the pain underneath the habit. Recovery is more likely when the root issues are acknowledged—not just the behaviour.
10. Their emotions may feel like they’re either all in or completely shut down.

Some veterans describe feeling emotionally numb, while others feel like their anger or sadness comes on too strong. This emotional swing can be confusing—not just for them, but for those around them. They need space to process these shifts without being told to “calm down” or “open up” on demand. Emotional regulation is a skill, and like any skill, it needs time, support, and practice.
11. Everyday situations can feel harder than they look.

Crowded places, loud noises, or unpredictable environments can be overwhelming. Even something as simple as grocery shopping or attending a social event might take a huge mental toll. They need people to understand that just because they look fine doesn’t mean they’re not pushing through something difficult. Small acts of patience and understanding can go a long way.
12. They need to be seen as more than what they’ve been through.
Veterans are more than trauma. They’re parents, artists, thinkers, leaders, and friends. Focusing only on their pain can be just as dehumanising as ignoring it completely. What they truly need is to be seen in full: not just as survivors, but as whole people who deserve joy, connection, and a future that feels like their own again.




